Our research within the Immunology Centre of Excellence focuses on the prevention and/or treatment of inflammation, allergy, infections and/or non-communicable diseases in later life. Our mission can only be reached with a solid pre-clinical research program, using state-of-the-art in vitro, in vivo and ex vivo techniques. In addition, we are closely involved in the design, measurements and interpretation of immunological data from clinical studies. We develop and execute many of this work in collaboration with national and international academic, industrial and governmental partners.

With 40 years of innovation and scientific discoveries and more than 600 publications in peer-reviewed journals in the field of immunology, we are committed to deliver high-quality, safe nutrition. We use a range of research tools, from preclinical studies to proof of concept and multicenter, efficacy clinical studies, and collaborate closely with both national and international academic partners and healthcare providers.
Allergy research
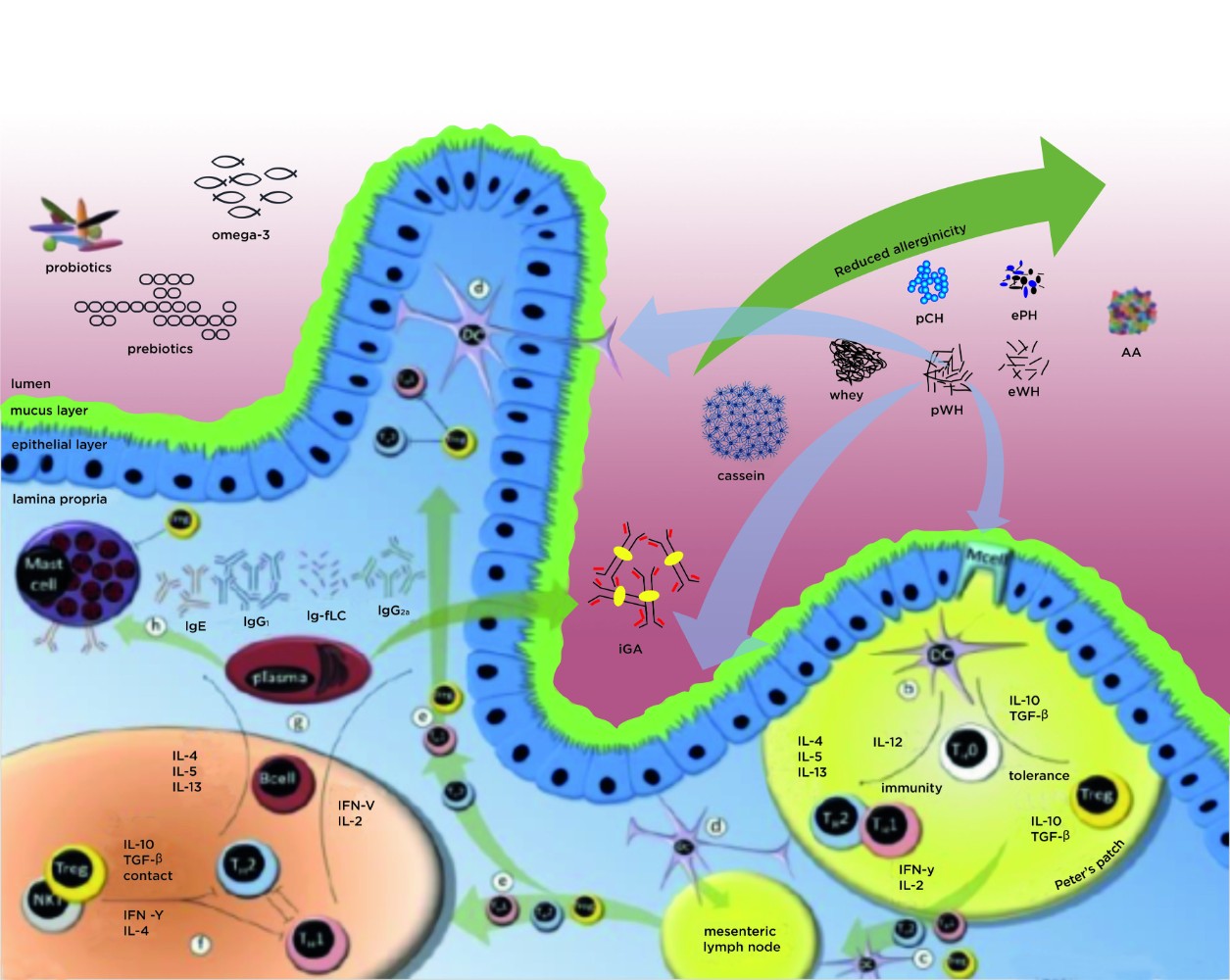
Allergy is directly related to the immune system, and as such is referred to as an ‘immune-mediated’ disease. To increase our understanding of the mechanisms underlying allergy development, improve treatment options and better understand the influence of nutrition in this process, we have a large pre-clinical allergy programme.

General Immune modulation
We investigate the underlying mechanisms behind the immune modulation and prevention of allergy with pre-, pro- and synbiotics, the effectiveness of allergy treatment and the induction of tolerance to harmless antigens.
Tolerance development
Until recently, the focus of allergy management has been on allergen avoidance. Infants with cow’s milk allergy are advised to eliminate cow’s milk from their diet. If this does not resolve the allergy, infants are given formula that is free of cow’s milk proteins, existing of hydrolysed proteins (peptides) or amino acids in very severe cases., Next to the proven efficacy of avoidance in severe cases of cow’s milk allergy, there is now increasing evidence that supports the benefit of controlled exposure to allergens, leading to the development of tolerance against harmless antigens. At Danone Research & Innovation, we have an extensive pre-clinical research programme focusing on tolerance development in both the allergy prevention and management setting.
Environmental challenges
It is thought the rising allergy epidemic is due to the vulnerability of the developing immune system to challenges related to modern life,1 including pollution, the use of antibiotics and C-section deliveries. We are investigating the effects of pollution on the developing immune system and how this influences the development of diseases, such as allergy.

New ingredients and immune development
We work hard on identifying and unravelling the mechanisms behind new nutritional components, such as pre-, pro-, syn- and postbiotics, human milk oligosaccharides and amino acids, that could positively influence immune development and the active immune response. We investigate the effects of these ingredients on the development of infections, autoimmune disorders and allergy.

Inflammation management
One of the crucial determinants of immune fitness is the ability to manage inflammation. Inflammation is a necessary response of the immune system, predominantly to manage infections, however, chronic inflammation can lead to allergy or autoimmune disorders. We are investigating the effects of amino acids on inflammation development in allergy, mucositis and Inflammatory Bowel Disease.
Biomarker discovery, validation and measurement
To be able to unravel and understand the mechanisms of inflammation, immune development and the effects of ingredients, in both the pre-clinical as well as the clinical setting, it is crucial to know what to measure and how this correlates with prevention or treatment of disease. To further our understanding in this field, we have a large Biomarker Discovery program. In this program state-of-the-art techniques are used, such as proteomics, metabolomics and transcriptomics, in which we analyse large data sets using systems biology and machine learning approaches.

In addition, we assure the immune-related measurements performed in our clinical studies are fully validated according to ISO standards, so we can deliver high-quality results.
As an example of our discovery programme, we investigated the role of immunoglobulin free light chains (Ig-fLC) in several different inflammatory conditions. During the synthesis of immunoglobulins, Ig-fLCs are produced in excess over heavy chains and they might play a crucial role in the pathogenesis of inflammatory disease, however, the exact mode of action is still unknown. We have demonstrated that in idiopathic pulmonary fibrosis and chronic hypersensitivity pneumonitis, both lung disorders, Ig-fLC concentrations are increased in serum and broncho-alveleor lavage fluid of these patients and that Ig-fLCs are present within affected lung tissue.1Groot Kormelink T, et al. PLoS ONE. Published on 2011;6(9):e25392
In eosinophilic oesophagitis (EoE), an allergic disorder associated with male gender was found that serum Ig-fLC appeared higher in females than in males, adding another gender difference to the biology of EoE.2Knipping K, et al. Acta Paediatr. Published on 2014;103(7):766-74 Very recently we investigated whether Ig-fLCs could be a marker for disease severity in adult atopic dermatitis patients. Although serum concentrations were high, no differences in concentrations were found in patients before and after treatment of the atopic dermatitis.3Thijs JL, et al. Clin Transl Allergy. Published on 2016;6:44 This indicates that Ig-fLC indeed seems to play a role in inflammatory diseases but the mechanism still has to be unraveled.